Identification
- Summary
Insulin human is a recombinant form of human insulin used to control hyperglycemia in diabetes mellitus.
- Brand Names
- Actraphane, Actrapid, Afrezza, Entuzity, Exubera, Humulin, Humulin N, Humulin R, Insulatard, Insuman, Myxredlin, Novolin, Novolin N, Novolin R
- Generic Name
- Insulin human
- DrugBank Accession Number
- DB00030
- Background
Human Insulin, also known as Regular Insulin, is a short-acting form of insulin used for the treatment of hyperglycemia caused by Type 1 and Type 2 Diabetes. Human insulin is produced by recombinant DNA technology and is identical to endogenously produced insulin. Typically prescribed for the management of diabetes mellitus, insulin is a peptide hormone produced by beta cells of the pancreas that promotes glucose metabolism. Insulin is released from the pancreas following a meal to promote the uptake of glucose from the blood into internal organs and tissues such as the liver, fat cells, and skeletal muscle. Absorption of glucose into cells allows for its transformation into glycogen or fat for storage. Insulin also inhibits hepatic glucose production, enhances protein synthesis, and inhibits lipolysis and proteolysis among many other functions.
Insulin is an important treatment in the management of Type 1 Diabetes (T1D) which is caused by an autoimmune reaction that destroys the beta cells of the pancreas, resulting in the body not being able to produce or synthesize the insulin needed to manage circulating blood sugar levels. As a result, people with T1D rely primarily on exogenous forms of insulin to lower glucose levels in the blood. Insulin is also used in the treatment of Type 2 Diabetes (T2D), another form of diabetes mellitus that is a slowly progressing metabolic disorder caused by a combination of genetic and lifestyle factors that promote chronically elevated blood sugar levels. Without treatment or improvement in non-pharmacological measures such as diet and exercise to lower blood glucose, high blood sugar eventually causes cellular resistance to endogenous insulin, and in the long term, damage to pancreatic islet cells. Insulin is typically prescribed later in the course of T2D, after trying several oral medications such as Metformin, Gliclazide, or Sitagliptin have been tried, when sufficient damage has been caused to pancreatic cells that the body is no longer able to produce insulin on its own.
Marketed as the brand name product Humulin R or Novolin R, human insulin begins to exert its effects within 30 minutes of subcutaneous administration, while peak levels occur 3-4 hours after administration. Due to its quick onset of action, human insulin is considered "bolus insulin" as it provides high levels of insulin in a short period of time to mimic the release of endogenous insulin from the pancreas after meals. Bolus insulin is often combined with once daily, long-acting "basal insulin" such as Insulin detemir, Insulin degludec, and Insulin glargine to provide low concentrations of background insulin that can keep blood sugar stable between meals or overnight. Use of basal and bolus insulin together is intended to mimic the pancreas' production of endogenous insulin, with a goal of avoiding any periods of hypoglycemia.
Human insulin is also available in an inhalable form, intended to be used as a bolus meal-time insulin. Exubera was the first inhaled insulin available on the market and was developed by Inhale Therapeutics (later named Nektar Therapeutics). Unfortunately, limited uptake by physicians and patients, poor sales, bulky packaging, and concerns over the possible impact on lung cancer development resulted in Exubera products being withdrawn from the US markets 6. Exubera was followed by Afrezza, a monomeric inhaled insulin developed by Mannkind Corporation, which received FDA approval in 2016. While still available in the US, Afrezza has had similar concerns associated with its use, and had an FDA "black box" warning added to it to warn about use in patients with chronic lung disease. Afrezza does not currently have Health Canada or European Medicines Agency approval for marketing in Canada or the EU.
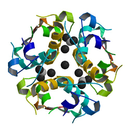
Human Insulin is a 51 residue peptide hormone produced by recombinant DNA technology by inserting the human insulin gene into Escherichia coli bacteria or Saccharomyces cerevisiae. The structure is identical to native human insulin, with two amino acid chains covalently linked by disulfide bonds.
Human insulin is also available in an intermediate-acting form as NPH (Neutral Protamine Hagedorn) as the marketed products Novolin N and Humulin N. NPH insulin is provided as a crystalline suspension of insulin with protamine and zinc, resulting in an onset of action in 1 to 3 hours, duration of action up to 24 hours, and peak action from 6 to 8 hours. Due to the added crystals, NPH insulin is typically cloudy when compared to other forms of insulin and has a neutral pH.
Without an adequate supply of insulin to promote absorption of glucose from the bloodstream, blood sugar levels can climb to dangerously high levels and can result in symptoms such as fatigue, headache, blurred vision, and increased thirst. If left untreated, the body starts to break down fat, instead of glucose, for energy which results in a build-up of ketone acids in the blood and a syndrome called ketoacidosis, which is a life-threatening medical emergency. In the long term, elevated blood sugar levels increase the risk of heart attack, stroke, and diabetic neuropathy.
- Type
- Biotech
- Groups
- Approved, Investigational
- Biologic Classification
- Protein Based Therapies
Hormones / Insulins - Protein Structure
- Protein Chemical Formula
- C257H383N65O77S6
- Protein Average Weight
- 5808.0 Da
- Sequences
- Synonyms
- High molecular weight insulin human
- Human insulin
- human insulin (rDNA)
- Insulin (human)
- Insulin human
- Insulin human [rDNA origin]
- Insulin Human Regular
- Insulin human regular (rDNA)
- Insulin human, rDNA origin
- Insulin recombinant human
- Insulin recombinant purified human
- Insulin regular
- Insulin, human
- Insulina regular
- Neutral insulin
- Regular Insulin, human
- Soluble insulin
Pharmacology
- Indication
Human insulin is indicated to improve glycemic control in adults and pediatric patients with diabetes mellitus.
 Reduce drug development failure ratesBuild, train, & validate machine-learning modelswith evidence-based and structured datasets.Build, train, & validate predictive machine-learning models with structured datasets.
Reduce drug development failure ratesBuild, train, & validate machine-learning modelswith evidence-based and structured datasets.Build, train, & validate predictive machine-learning models with structured datasets.- Associated Conditions
Indication Type Indication Combined Product Details Approval Level Age Group Patient Characteristics Dose Form Management of Diabetes mellitus ••• ••• •••••• •••••••• ••••••••••••••••• ••••••••• Management of Diabetes mellitus ••• ••• •••••• •••••••• ••••••••• Management of Diabetes mellitus ••• ••• •••••• •••••••• •••••••••• •••••••• Management of Diabetes mellitus ••• ••• •••••• •••••••• •••••••••• •••••••• Management of Diabetes mellitus •••••••••••• ••••• •••••••• •••••• - Contraindications & Blackbox Warnings
 Prevent Adverse Drug Events TodayTap into our Clinical API for life-saving information on contraindications & blackbox warnings, population restrictions, harmful risks, & more.Avoid life-threatening adverse drug events with our Clinical API
Prevent Adverse Drug Events TodayTap into our Clinical API for life-saving information on contraindications & blackbox warnings, population restrictions, harmful risks, & more.Avoid life-threatening adverse drug events with our Clinical API- Pharmacodynamics
Insulin is a natural hormone produced by beta cells of the pancreas. In non-diabetic individuals, a basal level of insulin is supplemented with insulin spikes following meals. Postprandial insulin spikes are responsible for the metabolic changes that occur as the body transitions from a postabsorptive to absorptive state. Insulin promotes cellular uptake of glucose, particularly in muscle and adipose tissues, promotes energy storage via glycogenesis, opposes catabolism of energy stores, increases DNA replication and protein synthesis by stimulating amino acid uptake by liver, muscle and adipose tissue, and modifies the activity of numerous enzymes involved in glycogen synthesis and glycolysis. Insulin also promotes growth and is required for the actions of growth hormone (e.g. protein synthesis, cell division, DNA synthesis).
- Mechanism of action
The primary activity of insulin is the regulation of glucose metabolism. Insulin promotes glucose and amino acid uptake into muscle and adipose tissues, and other tissues except brain and liver. It also has an anabolic role in stimulating glycogen, fatty acid, and protein synthesis. Insulin inhibits gluconeogenesis in the liver. Insulin binds to the insulin receptor (IR), a heterotetrameric protein consisting of two extracellular alpha units and two transmembrane beta units. The binding of insulin to the alpha subunit of IR stimulates the tyrosine kinase activity intrinsic to the beta subunit of the receptor. The bound receptor is able to autophosphorylate and phosphorylate numerous intracellular substrates such as insulin receptor substrates (IRS) proteins, Cbl, APS, Shc and Gab 1. These activated proteins, in turn, lead to the activation of downstream signaling molecules including PI3 kinase and Akt. Akt regulates the activity of glucose transporter 4 (GLUT4) and protein kinase C (PKC) which play a critical role in metabolism and catabolism.
Target Actions Organism AInsulin receptor agonistHumans UInsulin-like growth factor 1 receptor activatorHumans UCarboxypeptidase E modulatorproduct ofHumans UProtein NOV homolog downregulatorHumans ULow-density lipoprotein receptor-related protein 2 substrateHumans UInsulin-like growth factor-binding protein 7 inhibitorbinderHumans - Absorption
When injected subcutaneously, the glucose-lowering effect of human insulin begins approximately 30 minutes post-dose. After a single subcutaneous administration of 0.1 unit/kg of human insulin to healthy subjects, peak insulin concentrations occurred between 1.5 to 2.5 hours post-dose.
When administered in an inhaled form (as the product Afrezza), the time to maximum serum insulin concentration ranges from 10-20 minutes after oral inhalation of 4 to 48 units of human insulin. Serum insulin concentrations declined to baseline by approximately 60-240 minutes for these dose levels. Intrapatient variability in insulin exposure measured by AUC and Cmax is approximately 16% (95% CI 12-23%) and 21% (95% CI 16-30%), respectively.
- Volume of distribution
Not Available
- Protein binding
Not Available
- Metabolism
The metabolism and elimination of orally inhaled human insulin are comparable to regular human insulin.
- Route of elimination
Following oral inhalation of human insulin, a mean of 39% of the inhaled dose of carrier particles was distributed to the lungs and a mean of 7% of the dose was swallowed. The swallowed fraction was not absorbed from the GI tract and was eliminated unchanged in the feces.
- Half-life
Systemic insulin disposition (apparent terminal half-life) following oral inhalation of 4 to 48 units of human insulin was 120-206 minutes.
- Clearance
Not Available
- Adverse Effects
 Improve decision support & research outcomesWith structured adverse effects data, including: blackbox warnings, adverse reactions, warning & precautions, & incidence rates. View sample adverse effects data in our new Data Library!Improve decision support & research outcomes with our structured adverse effects data.
Improve decision support & research outcomesWith structured adverse effects data, including: blackbox warnings, adverse reactions, warning & precautions, & incidence rates. View sample adverse effects data in our new Data Library!Improve decision support & research outcomes with our structured adverse effects data.- Toxicity
Not Available
- Pathways
- Not Available
- Pharmacogenomic Effects/ADRs
- Not Available
Interactions
- Drug Interactions
- This information should not be interpreted without the help of a healthcare provider. If you believe you are experiencing an interaction, contact a healthcare provider immediately. The absence of an interaction does not necessarily mean no interactions exist.
Drug Interaction Integrate drug-drug
interactions in your softwareAcarbose The risk or severity of hypoglycemia can be increased when Acarbose is combined with Insulin human. Acebutolol The therapeutic efficacy of Insulin human can be increased when used in combination with Acebutolol. Acetazolamide The risk or severity of hypoglycemia can be increased when Acetazolamide is combined with Insulin human. Acetohexamide The risk or severity of hypoglycemia can be increased when Acetohexamide is combined with Insulin human. Acetophenazine The therapeutic efficacy of Insulin human can be decreased when used in combination with Acetophenazine. - Food Interactions
- Avoid alcohol. Alcohol may impair blood glucose control.
Products
 Drug product information from 10+ global regionsOur datasets provide approved product information including:dosage, form, labeller, route of administration, and marketing period.Access drug product information from over 10 global regions.
Drug product information from 10+ global regionsOur datasets provide approved product information including:dosage, form, labeller, route of administration, and marketing period.Access drug product information from over 10 global regions.- Product Ingredients
Ingredient UNII CAS InChI Key Insulin human zinc suspension Not Available Not Available Not applicable NPH insulin Not Available 53027-39-7 Not applicable - Brand Name Prescription Products
Name Dosage Strength Route Labeller Marketing Start Marketing End Region Image Actraphane 30 Injection, suspension 40 iu/ml Subcutaneous Novo Nordisk 2016-09-07 Not applicable EU Actraphane 30 Injection, suspension 100 iu/ml Subcutaneous Novo Nordisk 2016-09-07 Not applicable EU Actraphane 30 Injection, suspension 100 iu/ml Subcutaneous Novo Nordisk 2016-09-07 Not applicable EU Actraphane 30 Injection, suspension 40 iu/ml Subcutaneous Novo Nordisk 2016-09-07 Not applicable EU Actraphane 30 Injection, suspension 100 iu/ml Subcutaneous Novo Nordisk 2016-09-07 Not applicable EU - Over the Counter Products
Name Dosage Strength Route Labeller Marketing Start Marketing End Region Image ACTRAPID INJECTION 100 IU/ml Injection 100 IU/ml Intramuscular; Intravenous; Subcutaneous NOVO NORDISK PHARMA (SINGAPORE) PTE LTD 1988-11-24 Not applicable Singapore ACTRAPID PENFILL INJECTION 100 IU/ml Injection 100 iu/ml Subcutaneous NOVO NORDISK PHARMA (SINGAPORE) PTE LTD 1988-11-24 Not applicable Singapore Humalog 70/30 Injection, suspension 100 [iU]/1mL Subcutaneous Physicians Total Care, Inc. 1994-12-28 Not applicable US Humulin 50/50 Injection, suspension 100 [iU]/1mL Subcutaneous Eli Lilly & Co. Ltd. 1992-05-18 2010-05-31 US Humulin 70/30 Injection, suspension 100 [iU]/1mL Subcutaneous A-S Medication Solutions 1989-06-26 Not applicable US - Mixture Products
Name Ingredients Dosage Route Labeller Marketing Start Marketing End Region Image ACTRAPHANE 30 FLEXPEN Insulin human (30 IU/mL) + NPH insulin (70 IU/ml) Injection, suspension Parenteral 2015-04-01 Not applicable Germany ACTRAPHANE 30 FLEXPEN Insulin human (30 IU/mL) + NPH insulin (70 IU/ml) Injection, suspension Parenteral 2015-04-01 Not applicable Germany ACTRAPHANE 30 FLEXPEN Insulin human (30 IU/mL) + NPH insulin (70 IU/ml) Injection, suspension Parenteral 2015-04-01 Not applicable Germany ACTRAPHANE 30 FLEXPEN Insulin human (30 IU/mL) + NPH insulin (70 IU/ml) Injection, suspension Parenteral 2015-04-01 Not applicable Germany ACTRAPHANE 30 INNOLET FER Insulin human (30 IU/mL) + NPH insulin (70 IU/ml) Injection, suspension Parenteral 2015-04-01 Not applicable Germany
Categories
- ATC Codes
- A10AC01 — Insulin (human)
- A10AC — Insulins and analogues for injection, intermediate-acting
- A10A — INSULINS AND ANALOGUES
- A10 — DRUGS USED IN DIABETES
- A — ALIMENTARY TRACT AND METABOLISM
- A10AE — Insulins and analogues for injection, long-acting
- A10A — INSULINS AND ANALOGUES
- A10 — DRUGS USED IN DIABETES
- A — ALIMENTARY TRACT AND METABOLISM
- A10AB — Insulins and analogues for injection, fast-acting
- A10A — INSULINS AND ANALOGUES
- A10 — DRUGS USED IN DIABETES
- A — ALIMENTARY TRACT AND METABOLISM
- A10AD — Insulins and analogues for injection, intermediate- or long-acting combined with fast-acting
- A10A — INSULINS AND ANALOGUES
- A10 — DRUGS USED IN DIABETES
- A — ALIMENTARY TRACT AND METABOLISM
- Drug Categories
- Alimentary Tract and Metabolism
- Amino Acids, Peptides, and Proteins
- Blood Glucose Lowering Agents
- Cytochrome P-450 CYP1A2 Inducers
- Cytochrome P-450 CYP1A2 Inducers (strength unknown)
- Cytochrome P-450 Enzyme Inducers
- Drugs Used in Diabetes
- Hormones
- Hormones, Hormone Substitutes, and Hormone Antagonists
- Hypoglycemia-Associated Agents
- Insulin
- Insulin, metabolism
- Insulin, Short-Acting
- Insulins and Analogues for Injection, Fast-Acting
- Pancreatic Hormones
- Peptide Hormones
- Peptides
- Chemical TaxonomyProvided by Classyfire
- Description
- Not Available
- Kingdom
- Organic Compounds
- Super Class
- Organic Acids
- Class
- Carboxylic Acids and Derivatives
- Sub Class
- Amino Acids, Peptides, and Analogues
- Direct Parent
- Peptides
- Alternative Parents
- Not Available
- Substituents
- Not Available
- Molecular Framework
- Not Available
- External Descriptors
- Not Available
- Affected organisms
- Humans and other mammals
Chemical Identifiers
- UNII
- 1Y17CTI5SR
- CAS number
- 11061-68-0
References
- Synthesis Reference
Humulin is synthesized in a special non-disease-producing laboratory strain of Escherichia coli bacteria that has been genetically altered to produce human insulin.
- General References
- Herrmann BL, Kasser C, Keuthage W, Huptas M, Dette H, Klute A: Comparison of insulin aspart vs. regular human insulin with or without insulin detemir concerning adipozytokines and metabolic effects in patients with type 2 diabetes mellitus. Exp Clin Endocrinol Diabetes. 2013 Apr;121(4):210-3. doi: 10.1055/s-0033-1334905. Epub 2013 Mar 19. [Article]
- Lepore M, Pampanelli S, Fanelli C, Porcellati F, Bartocci L, Di Vincenzo A, Cordoni C, Costa E, Brunetti P, Bolli GB: Pharmacokinetics and pharmacodynamics of subcutaneous injection of long-acting human insulin analog glargine, NPH insulin, and ultralente human insulin and continuous subcutaneous infusion of insulin lispro. Diabetes. 2000 Dec;49(12):2142-8. [Article]
- Owens DR, Coates PA, Luzio SD, Tinbergen JP, Kurzhals R: Pharmacokinetics of 125I-labeled insulin glargine (HOE 901) in healthy men: comparison with NPH insulin and the influence of different subcutaneous injection sites. Diabetes Care. 2000 Jun;23(6):813-9. [Article]
- Danne T, Lupke K, Walte K, Von Schuetz W, Gall MA: Insulin detemir is characterized by a consistent pharmacokinetic profile across age-groups in children, adolescents, and adults with type 1 diabetes. Diabetes Care. 2003 Nov;26(11):3087-92. [Article]
- Owens DR, Bolli GB: Beyond the era of NPH insulin--long-acting insulin analogs: chemistry, comparative pharmacology, and clinical application. Diabetes Technol Ther. 2008 Oct;10(5):333-49. doi: 10.1089/dia.2008.0023. [Article]
- Oleck J, Kassam S, Goldman JD: Commentary: Why Was Inhaled Insulin a Failure in the Market? Diabetes Spectr. 2016 Aug;29(3):180-4. doi: 10.2337/diaspect.29.3.180. [Article]
- FDA Approved Drug Products: Humulin R (insulin human) [Link]
- FDA Approved Drug Products: AFREZZA® (insulin human) inhalation powder, for oral inhalation use (February 2023) [Link]
- FDA Approved Drug Products: AFREZZA (insulin human) Inhalation Powder [Link]
- External Links
- UniProt
- Q8HXV2
- Genbank
- AY137503
- KEGG Drug
- D03230
- KEGG Compound
- C00723
- PubChem Substance
- 46506231
- 253182
- ChEBI
- 5931
- Therapeutic Targets Database
- DAP000802
- PharmGKB
- PA164744571
- RxList
- RxList Drug Page
- Drugs.com
- Drugs.com Drug Page
- Wikipedia
- Insulin
- FDA label
- Download (828 KB)
- MSDS
- Download (47 KB)
Clinical Trials
- Clinical Trials
Phase Status Purpose Conditions Count 4 Active Not Recruiting Treatment Colorectal Cancer 1 4 Active Not Recruiting Treatment Diabetes Related Cystic Fibrosis 1 4 Active Not Recruiting Treatment Type 1 Diabetes Mellitus 1 4 Completed Not Available Cirrhosis of the Liver / Diabetes Mellitus 1 4 Completed Not Available Polycystic Ovarian Syndrome (PCOS) 1
Pharmacoeconomics
- Manufacturers
- Novo nordisk inc
- Packagers
- A-S Medication Solutions LLC
- DispenseXpress Inc.
- Eli Lilly & Co.
- Hospira Inc.
- Intervet International
- Novo Nordisk Inc.
- Pfizer Inc.
- Physicians Total Care Inc.
- Dosage Forms
Form Route Strength Injection, suspension Cutaneous; Parenteral 100 IU/ml Injection, suspension Cutaneous; Parenteral 40 IU/ml Injection, suspension Parenteral; Subcutaneous 100 IU/ml Injection, suspension Parenteral; Subcutaneous 100 UI/ML Injection, suspension Parenteral; Subcutaneous 40 UI/ML Injection, suspension Parenteral Injection, solution Intravenous; Parenteral 100 IU/ML Injection, solution Intravenous; Parenteral 40 IU/ML Injection, solution Intravenous; Subcutaneous 100 IU/ML Injection, solution Intravenous; Subcutaneous 40 iu/ml Injection, solution Parenteral; Subcutaneous 100 IU/ML Solution Subcutaneous Injection, solution Parenteral 100 IU/mL Injection Injection Intramuscular; Intravenous; Subcutaneous 100 IU/ml Injection, solution Parenteral 100 IE Injection, solution Parenteral 100 IE/ML Injection, solution Parenteral 100 I.E./ML Solution Subcutaneous 100 IU/ml Solution 100 IU/ml Kit Respiratory (inhalation) Powder, metered Respiratory (inhalation) 12 [arb'U]/1 Powder, metered Respiratory (inhalation) 4 1/1 Powder, metered Respiratory (inhalation) 4 [arb'U]/1 Powder, metered Respiratory (inhalation) 8 1/1 Powder, metered Respiratory (inhalation) 8 [arb'U]/1 Injection, suspension Parenteral 3 ML Injection, solution Parenteral 3 ML Injection, suspension Subcutaneous Injection, suspension 100 iu/1ml Solution Subcutaneous 500 unit / mL Aerosol, powder Respiratory (inhalation) 1 mg/1 Aerosol, powder Respiratory (inhalation) 3 mg/1 Injection Parenteral Injection, solution Subcutaneous Injection, solution Injection, suspension Parenteral 100 IU Injection, suspension Parenteral 1000 IU Injection, solution Parenteral 100 IU Injection, solution Intravenous 100 IU/ML Injection, solution Subcutaneous 100 IU/ML Injection, suspension Subcutaneous 100 units/mL Injection, suspension Subcutaneous 40 units/mL Suspension Subcutaneous Injection Intramuscular; Subcutaneous Injection, suspension Injection, suspension Subcutaneous 100 [iU]/1mL Injection, suspension Subcutaneous 100 Injection, suspension Parenteral 300 IU Suspension Subcutaneous 100 unit/mL Suspension Subcutaneous 100 unit / mL Injection Intramuscular; Subcutaneous 100 iu/ml Injection, solution Parenteral 300 IU Injection, solution Parenteral 100 [iU]/1mL Injection, solution Subcutaneous 100 [iU]/1mL Solution Intramuscular; Intravenous; Subcutaneous 100 unit/mL Solution Subcutaneous 100 UI Solution Intramuscular; Subcutaneous 100 unit/mL Injection, solution Subcutaneous 500 [iU]/1mL Injection, solution Intravenous 1 UI/mL Injection, solution Intravenous 1 IU/ml Injection 100 iu/ml Injection, suspension Parenteral 100 IE/ML Injection Subcutaneous 100 IU/ml Injection, suspension Subcutaneous 30 iu/1mL Suspension Intramuscular; Subcutaneous 100 IU Solution Subcutaneous 100 IU Solution Parenteral 100.000 UI Injection, solution Intramuscular; Parenteral 100 IU/ML Injection, solution Intravenous; Parenteral 100 UI/ML Injection, solution Parenteral; Subcutaneous 100 UI/ML Injection, solution Parenteral; Subcutaneous 40 UI/ML Injection, suspension Intramuscular 100 IU/ml Injection, suspension Intramuscular 40 IU/ml Injection, suspension Intramuscular; Subcutaneous 100 IU/ml Injection, suspension Subcutaneous 100 UI/ML Injection, suspension Subcutaneous 40 IU/ml Injection, suspension Subcutaneous 40 UI/ML Solution Subcutaneous 100 UI/ML Solution Subcutaneous 40 UI/ML Suspension Injection, suspension Parenteral 100 I.E./ML Injection, suspension Parenteral 40 IE/ML Injection Subcutaneous Injection, suspension Parenteral 100 IE Suspension Subcutaneous Injection, solution Intraperitoneal 400 IU/ml Injection, solution Parenteral 40 IE/ML Injection, solution 100 iu/ml Injection; injection, solution 100 IU/ml Injection 300 IU/ml Injection Subcutaneous Injection Subcutaneous 70 IU/ml Injection, suspension Parenteral 100 IU/ml Injection, suspension Subcutaneous Injection, suspension Subcutaneous 100 IU/ml Suspension 100 IU/ml Injection, solution Intravenous 1.00 [iU]/1mL Solution Intravenous 1 unit / mL Injection, suspension Subcutaneous 100 [USP'U]/1mL Solution Intramuscular; Intravenous; Subcutaneous 100 unit / mL Solution Other 100 UI Solution Intravenous; Subcutaneous 100 IU Liquid Intramuscular; Intravenous; Subcutaneous 100 unit / mL Injection, suspension Parenteral; Subcutaneous 40 IU/ML Injection, suspension Parenteral 100 UI/ml Solution Intramuscular; Intravenous; Subcutaneous 100 IU Suspension Subcutaneous 100 IU Solution Parenteral 100 UI Suspension Parenteral 100 UI Injection, suspension Suspension Suspension 100 iu/1ml Injection, solution 100 iu/1ml Solution 100 iu/1ml - Prices
Unit description Cost Unit NovoLIN R PenFill 100 unit/ml Solution Five 3ml Cartridges Per Box = 15ml 162.26USD cartridge NovoLIN R 100 unit/ml Solution 10ml Vial 73.19USD vial Novolin r 100 unit/ml cartridg 33.33USD ml NovoLIN R InnoLet 100 unit/ml Solution 3ml Cartridge 24.17USD cartridge Humulin N Cartridge 100 unit/ml Cartridge 2.99USD cartridge Humulin R Cartridge 100 unit/ml Cartridge 2.99USD cartridge Novolin Ge Toronto Penfill 100 unit/ml Cartridge 2.8USD cartridge Novolin Ge Nph Penfill 100 unit/ml Cartridge 2.78USD cartridge Humulin N 100 unit/ml 2.29USD cartridge Humulin R 100 unit/ml 2.29USD cartridge Novolin Ge Nph 100 unit/ml 2.14USD cartridge Novolin Ge Toronto 100 unit/ml 2.14USD cartridge DrugBank does not sell nor buy drugs. Pricing information is supplied for informational purposes only.- Patents
Patent Number Pediatric Extension Approved Expires (estimated) Region USRE37872 No 2002-10-08 2010-02-12 US CA2183577 No 2007-10-30 2015-02-07 Canada CA2253393 No 2007-10-09 2017-05-07 Canada US7291132 No 2007-11-06 2024-08-09 US US6257233 No 2001-07-10 2019-05-14 US US6546929 No 2003-04-15 2019-05-14 US US6685967 No 2004-02-03 2018-09-11 US US6582728 No 2003-06-24 2020-06-24 US US8912193 No 2014-12-16 2029-06-12 US US7648960 No 2010-01-19 2020-06-29 US US6652885 No 2003-11-25 2020-06-29 US US8258095 No 2012-09-04 2029-08-11 US US8778403 No 2014-07-15 2030-06-11 US US6444226 No 2002-09-03 2020-06-29 US US7943572 No 2011-05-17 2026-08-10 US US8119593 No 2012-02-21 2029-08-11 US US7943178 No 2011-05-17 2020-06-29 US US8889099 No 2014-11-18 2020-06-29 US US8623817 No 2014-01-07 2029-09-18 US US8389470 No 2013-03-05 2020-06-29 US US9192675 No 2015-11-24 2029-06-12 US US8215300 No 2012-07-10 2022-11-24 US US8146588 No 2012-04-03 2023-04-24 US US8950397 No 2015-02-10 2021-07-20 US US8485180 No 2013-07-16 2030-03-25 US US9283193 No 2016-03-15 2026-09-14 US US8636001 No 2014-01-28 2032-07-12 US US8424518 No 2013-04-23 2031-10-17 US US8551528 No 2013-10-08 2030-06-11 US US7464706 No 2008-12-16 2023-03-02 US US8729019 No 2014-05-20 2028-12-26 US US7305986 No 2007-12-11 2023-01-16 US US8499757 No 2013-08-06 2032-02-19 US US8156936 No 2012-04-17 2023-01-16 US US8734845 No 2014-05-27 2030-06-11 US US8227409 No 2012-07-24 2031-03-08 US US9393372 No 2016-07-19 2029-07-04 US US9339615 No 2016-05-17 2029-10-20 US US9511198 No 2016-12-06 2030-02-16 US US9597374 No 2017-03-21 2031-10-08 US US9358352 No 2016-06-07 2031-02-15 US US9446133 No 2016-09-20 2029-06-12 US US9662461 No 2017-05-30 2029-06-12 US US9717689 No 2017-08-01 2026-09-14 US US9943571 No 2018-04-17 2029-08-11 US US10046031 No 2018-08-14 2029-08-11 US US10201672 No 2019-02-12 2030-08-02 US US10342938 No 2019-07-09 2029-06-12 US US10500159 No 2019-12-10 2030-11-02 US
Properties
- State
- Liquid
- Experimental Properties
Property Value Source melting point (°C) 81 °C Khachidze, D.G. et al., J. Biol. Phys. Chem. 1:64-67 (2001)
Targets

- Kind
- Protein
- Organism
- Humans
- Pharmacological action
- Yes
- Actions
- Agonist
- General Function
- Receptor signaling protein tyrosine kinase activity
- Specific Function
- Receptor tyrosine kinase which mediates the pleiotropic actions of insulin. Binding of insulin leads to phosphorylation of several intracellular substrates, including, insulin receptor substrates (...
- Gene Name
- INSR
- Uniprot ID
- P06213
- Uniprot Name
- Insulin receptor
- Molecular Weight
- 156331.465 Da
References
- Desbuquois B, Chauvet G, Kouach M, Authier F: Cell itinerary and metabolic fate of proinsulin in rat liver: in vivo and in vitro studies. Endocrinology. 2003 Dec;144(12):5308-21. Epub 2003 Sep 11. [Article]
- Chen LM, Yang XW, Tang JG: Acidic residues on the N-terminus of proinsulin C-Peptide are important for the folding of insulin precursor. J Biochem. 2002 Jun;131(6):855-9. [Article]
- Bell DS: Insulin therapy in diabetes mellitus: how can the currently available injectable insulins be most prudently and efficaciously utilised? Drugs. 2007;67(13):1813-27. [Article]
- Tanti JF, Jager J: Cellular mechanisms of insulin resistance: role of stress-regulated serine kinases and insulin receptor substrates (IRS) serine phosphorylation. Curr Opin Pharmacol. 2009 Dec;9(6):753-62. doi: 10.1016/j.coph.2009.07.004. Epub 2009 Aug 13. [Article]
- Chiu SL, Cline HT: Insulin receptor signaling in the development of neuronal structure and function. Neural Dev. 2010 Mar 15;5:7. doi: 10.1186/1749-8104-5-7. [Article]
- Chen X, Ji ZL, Chen YZ: TTD: Therapeutic Target Database. Nucleic Acids Res. 2002 Jan 1;30(1):412-5. [Article]
- De Meyts P: The Insulin Receptor and Its Signal Transduction Network . [Article]
- Kind
- Protein
- Organism
- Humans
- Pharmacological action
- Unknown
- Actions
- Activator
- General Function
- Protein tyrosine kinase activity
- Specific Function
- Receptor tyrosine kinase which mediates actions of insulin-like growth factor 1 (IGF1). Binds IGF1 with high affinity and IGF2 and insulin (INS) with a lower affinity. The activated IGF1R is involv...
- Gene Name
- IGF1R
- Uniprot ID
- P08069
- Uniprot Name
- Insulin-like growth factor 1 receptor
- Molecular Weight
- 154791.73 Da
References
- Weinstein D, Simon M, Yehezkel E, Laron Z, Werner H: Insulin analogues display IGF-I-like mitogenic and anti-apoptotic activities in cultured cancer cells. Diabetes Metab Res Rev. 2009 Jan;25(1):41-9. doi: 10.1002/dmrr.912. [Article]
- Werner H, Weinstein D, Yehezkel E, Laron Z: Controversies in the use of insulin analogues. Expert Opin Biol Ther. 2011 Feb;11(2):199-209. doi: 10.1517/14712598.2011.540233. [Article]
- Varewijck AJ, Janssen JA: Insulin and its analogues and their affinities for the IGF1 receptor. Endocr Relat Cancer. 2012 Sep 5;19(5):F63-75. doi: 10.1530/ERC-12-0026. Print 2012 Oct. [Article]
- Sarfstein R, Nagaraj K, LeRoith D, Werner H: Differential Effects of Insulin and IGF1 Receptors on ERK and AKT Subcellular Distribution in Breast Cancer Cells. Cells. 2019 Nov 23;8(12). pii: cells8121499. doi: 10.3390/cells8121499. [Article]
- Donner T, Sarkar S: Insulin - Pharmacology, Therapeutic Regimens, and Principles of Intensive Insulin Therapy . [Article]
- Kind
- Protein
- Organism
- Humans
- Pharmacological action
- Unknown
- Actions
- ModulatorProduct of
- General Function
- Zinc ion binding
- Specific Function
- Removes residual C-terminal Arg or Lys remaining after initial endoprotease cleavage during prohormone processing. Processes proinsulin.
- Gene Name
- CPE
- Uniprot ID
- P16870
- Uniprot Name
- Carboxypeptidase E
- Molecular Weight
- 53150.185 Da
References
- Liew CW, Assmann A, Templin AT, Raum JC, Lipson KL, Rajan S, Qiang G, Hu J, Kawamori D, Lindberg I, Philipson LH, Sonenberg N, Goldfine AB, Stoffers DA, Mirmira RG, Urano F, Kulkarni RN: Insulin regulates carboxypeptidase E by modulating translation initiation scaffolding protein eIF4G1 in pancreatic beta cells. Proc Natl Acad Sci U S A. 2014 Jun 3;111(22):E2319-28. doi: 10.1073/pnas.1323066111. Epub 2014 May 19. [Article]
- Kind
- Protein
- Organism
- Humans
- Pharmacological action
- Unknown
- Actions
- Downregulator
- General Function
- Notch binding
- Specific Function
- Immediate-early protein playing a role in various cellular processes including proliferation, adhesion, migration, differentiation and survival (PubMed:15181016, PubMed:15611078, PubMed:12695522, P...
- Gene Name
- NOV
- Uniprot ID
- P48745
- Uniprot Name
- Protein NOV homolog
- Molecular Weight
- 39161.82 Da
References
- Paradis R, Lazar N, Antinozzi P, Perbal B, Buteau J: Nov/Ccn3, a novel transcriptional target of FoxO1, impairs pancreatic beta-cell function. PLoS One. 2013 May 21;8(5):e64957. doi: 10.1371/journal.pone.0064957. Print 2013. [Article]
- Kind
- Protein
- Organism
- Humans
- Pharmacological action
- Unknown
- Actions
- Substrate
- General Function
- Calcium ion binding
- Specific Function
- Acts together with cubilin to mediate HDL endocytosis (By similarity). May participate in regulation of parathyroid-hormone and para-thyroid-hormone-related protein release.
- Gene Name
- LRP2
- Uniprot ID
- P98164
- Uniprot Name
- Low-density lipoprotein receptor-related protein 2
- Molecular Weight
- 521952.77 Da
References
- Orlando RA, Rader K, Authier F, Yamazaki H, Posner BI, Bergeron JJ, Farquhar MG: Megalin is an endocytic receptor for insulin. J Am Soc Nephrol. 1998 Oct;9(10):1759-66. [Article]
- Kind
- Protein
- Organism
- Humans
- Pharmacological action
- Unknown
- Actions
- InhibitorBinder
- General Function
- Not Available
- Specific Function
- Binds IGF-I and IGF-II with a relatively low affinity. Stimulates prostacyclin (PGI2) production. Stimulates cell adhesion.
- Gene Name
- IGFBP7
- Uniprot ID
- Q16270
- Uniprot Name
- Insulin-like growth factor-binding protein 7
- Molecular Weight
- 29130.055 Da
References
- Radulescu RT: One for all and all for one: RB defends the cell while IDE, PTEN and IGFBP-7 antagonize insulin and IGFs to protect RB. Med Hypotheses. 2007;69(5):1018-20. Epub 2007 May 1. [Article]
Enzymes
- Kind
- Protein
- Organism
- Humans
- Pharmacological action
- Unknown
- Actions
- SubstrateCleavage
- General Function
- Zinc ion binding
- Specific Function
- Plays a role in the cellular breakdown of insulin, IAPP, glucagon, bradykinin, kallidin and other peptides, and thereby plays a role in intercellular peptide signaling. Degrades amyloid formed by A...
- Gene Name
- IDE
- Uniprot ID
- P14735
- Uniprot Name
- Insulin-degrading enzyme
- Molecular Weight
- 117967.49 Da
References
- Amata O, Marino T, Russo N, Toscano M: Human insulin-degrading enzyme working mechanism. J Am Chem Soc. 2009 Oct 21;131(41):14804-11. doi: 10.1021/ja9037142. [Article]
- Pivovarova O, von Loeffelholz C, Ilkavets I, Sticht C, Zhuk S, Murahovschi V, Lukowski S, Docke S, Kriebel J, de las Heras Gala T, Malashicheva A, Kostareva A, Lock JF, Stockmann M, Grallert H, Gretz N, Dooley S, Pfeiffer AF, Rudovich N: Modulation of insulin degrading enzyme activity and liver cell proliferation. Cell Cycle. 2015;14(14):2293-300. doi: 10.1080/15384101.2015.1046647. Epub 2015 May 6. [Article]
- Najjar SM, Perdomo G: Hepatic Insulin Clearance: Mechanism and Physiology. Physiology (Bethesda). 2019 May 1;34(3):198-215. doi: 10.1152/physiol.00048.2018. [Article]
- Kind
- Protein
- Organism
- Humans
- Pharmacological action
- Unknown
- Actions
- Activator
- General Function
- Serine-type endopeptidase activity
- Specific Function
- Involved in the processing of hormone and other protein precursors at sites comprised of pairs of basic amino acid residues. Responsible for the release of glucagon from proglucagon in pancreatic A...
- Gene Name
- PCSK2
- Uniprot ID
- P16519
- Uniprot Name
- Neuroendocrine convertase 2
- Molecular Weight
- 70564.735 Da
References
- Uniprot P16519 [Link]
- Kind
- Protein
- Organism
- Humans
- Pharmacological action
- Unknown
- Actions
- Activator
- General Function
- Serine-type endopeptidase activity
- Specific Function
- Involved in the processing of hormone and other protein precursors at sites comprised of pairs of basic amino acid residues. Substrates include POMC, renin, enkephalin, dynorphin, somatostatin, ins...
- Gene Name
- PCSK1
- Uniprot ID
- P29120
- Uniprot Name
- Neuroendocrine convertase 1
- Molecular Weight
- 84150.92 Da
References
- Uniprot P29120 [Link]
- Kind
- Protein
- Organism
- Humans
- Pharmacological action
- Unknown
- Actions
- Inducer
- General Function
- Oxidoreductase activity, acting on paired donors, with incorporation or reduction of molecular oxygen, reduced flavin or flavoprotein as one donor, and incorporation of one atom of oxygen
- Specific Function
- Cytochromes P450 are a group of heme-thiolate monooxygenases. In liver microsomes, this enzyme is involved in an NADPH-dependent electron transport pathway. It oxidizes a variety of structurally un...
- Gene Name
- CYP1A2
- Uniprot ID
- P05177
- Uniprot Name
- Cytochrome P450 1A2
- Molecular Weight
- 58293.76 Da
References
- Barnett CR, Wilson J, Wolf CR, Flatt PR, Ioannides C: Hyperinsulinaemia causes a preferential increase in hepatic P4501A2 activity. Biochem Pharmacol. 1992 Mar 17;43(6):1255-61. doi: 10.1016/0006-2952(92)90500-i. [Article]
- Pass GJ, Becker W, Kluge R, Linnartz K, Plum L, Giesen K, Joost HG: Effect of hyperinsulinemia and type 2 diabetes-like hyperglycemia on expression of hepatic cytochrome p450 and glutathione s-transferase isoforms in a New Zealand obese-derived mouse backcross population. J Pharmacol Exp Ther. 2002 Aug;302(2):442-50. doi: 10.1124/jpet.102.033553. [Article]
- Flockhart Table of Drug Interactions [Link]
Drug created at June 13, 2005 13:24 / Updated at February 20, 2024 23:55